Diarrhea and Dehydration 101
Stomach issues in kids aren’t fun, but being prepared can help ease the pain
An illness with many names
What do “stomach flu,” “pukey,” “stomach sick” and “the runs” all have in common? As parents, these terms bring a shiver to our spines, making us think of when our child has had a gastrointestinal illness causing vomiting and/or diarrhea. Pediatricians somewhat lovingly call this process “gastro,” which is short for gastroenteritis. All of us, parents and doctors alike, are referring to pretty much the same thing: it’s when someone catches a germ that rapidly changes our lives for a few days, and we count the seconds until it’s over.
What causes vomiting and diarrhea?
Gastroenteritis simply means an inflammatory process of the stomach and intestines that results vomiting and diarrhea. This is almost always caused by infections, either a virus or bacteria. While people label their illness as “food poisoning”, this is actually false, as modern food processing and delivery has essentially eliminated this once common cause. These days, nasty viruses and bacteria are usually passed directly from person to person. For example, after a person harboring the infection (prepare to cringe!!!) goes to the bathroom, contaminates their hands with the germ, doesn’t wash their hands properly, then touches another person or their food. These germs can also be spread by touching shared objects that were handled by contaminated hands, sharing cups and utensils, or sometimes by coughing in close proximity to another person. Sometimes there are large outbreaks of gastroenteritis from contaminated food that is mass produced, and we hear about these in the media every few months. Once a healthy person ingests or breathes in one of these nasty germs, then can get sick within a day or two… and the onset is generally FAST. [sigh]
How bad can it be?
Gastroenteritis hits you fast and furious. The good news is that the most severe symptoms, which include frequent vomiting and diarrhea episodes, often only lasts for the first day or two. However, gastroenteritis can be particularly dangerous for young children and infants, as these little humans can get dehydrated very quickly. When your child has gastroenteritis, the focus must be on keeping them hydrated. It takes a lot of work, but it is worth it!
Isn’t vomiting so much worse than diarrhea?
We all know that vomiting is very unpleasant. Indeed, there’s nothing quite like it. And as a parent of a child suffering from gastroenteritis, it is scary to see your child throw up everything that you just got them to finally drink. While the episodes of vomiting are tough on you and your child, this is actually your body’s way of trying to quickly get rid of the infection. Parents often worry about dehydration secondary to vomiting, but actually, a single episode of diarrhea actually causes the body to lose 3 to 4 times more fluid than a single episode of vomiting! So while we don’t want a child to vomit frequently as we’re trying to keep him or her hydrated, parents should focus their hydration efforts on preventing dehydration due to diarrhea.
So, what do I do when my kid has gastroenteritis?
Because gastroenteritis is usually caused by viruses, antibiotics are almost never needed to treat this infection. For some children with weakened immune systems, if a bacterial cause is found, antibiotics may be needed. Gastroenteritis will almost always resolve on its own without any specific treatments. However, parents must be diligent about keeping their children hydrated, and watch out for warning signs of dehydration. When your child has gastroenteritis, especially the first day, simply forget about food if your kid doesn’t want to eat-- it’s just not as important compared to hydration. Additionally, some foods can cause worsening of vomiting and diarrhea (and therefore causes losses of valuable fluids). FOCUS ON HYDRATION.
How do I keep my kid hydrated?
The best fluids to use to hydrate your child are low-sugar, electrolyte-rich fluids. Fluids high in sugar such as fruit juice and many sports drinks can actually be counterproductive, as the sugar can cause MORE diarrhea. An appropriate electrolyte-rich fluid to use is Pedialyte, which is an oral rehydration solution (ORS) that has the right balance of sugar and electrolytes. ORS can be made by you at home, which can save you both time, and money!
To make your own ORS, simply make a solution of 1 liter clean water + 6 level teaspoons of sugar + 1/2 level teaspoon of salt. Stir until the salt and sugar are dissolved, then the ORS is ready to use!
If your child will only drink juice, it’s important to dilute the juice with equal parts of water to avoid giving too much sugar. Water can also be used in the short term, but over time your child will need electrolytes for water to be absorbed. If your child takes formula or breastmilk, you should continue to try to use these fluids. Breast milk in particular is very easily digested. However, you’ll want to give very small amounts of fluid slowly. It’s always best to PREVENT dehydration rather than try to rehydrate later, so we recommend hydrating right off the bat if your child gets gastroenteritis.
Signs of dehydration
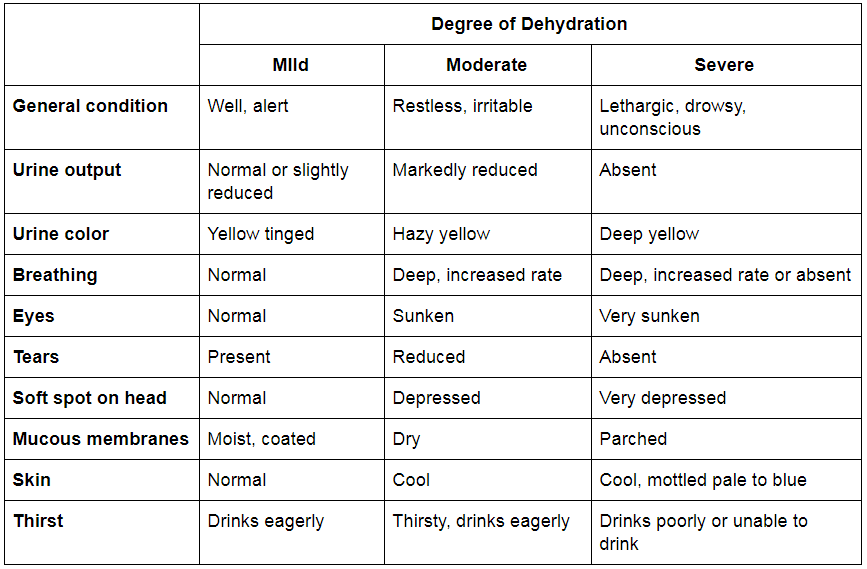
Dehydration is divided up into mild, moderate or severe. Mild dehydration can be managed at home. But especially with young children and infants, if your child is becoming moderately dehydrated, it’s best to involve your doctor in their care.
For a mildly dehydrated child, or a child who refuses to eat at home, here are some tips for hydrating your child. The goal is to replace your kid’s fluid deficit over a few hours, then replace what is lost with further vomiting and diarrhea.
Calculate how much your child needs now: for mild dehydration, a total of 5 teaspoons (which is the same as 25 milliliters and is close to 1 ounce) per pound of body weight.
Give fluids slowly, in 5mL increments at first, then up to 15 milliliters (half an ounce) at a time, which gives the stomach time to absorb fluids and avoid vomiting.
Use an oral syringe, spoon, bottle or cup, preferably one with measurement lines so you can keep track of how much you’ve given.
For every bout of diarrhea your child has, in addition to their usual intake, give infants up to 2 years 50-100 milliliters (or 2-3 ounces) in small increments as explained above; for children 2 years and older, give 100-200 milliliters (3-6 ounces) in small increments.
The child can return to their normal diet once they are no longer dehydrated. Keep giving extra fluids if your child's vomiting or diarrhea continues.
When do I need to seek medical care?
As we discussed earlier, most kids with mild dehydration can safely be managed at home with careful attention and encouraging increased fluid intake.
If your child has signs of moderate or severe dehydration, or you are unsure of what to do, we recommend you involve your doctor. If your child is difficult to arouse, is breathing fast or is struggling to breathe, or if they’re cool to the touch, you should urgently seek medical care or consider calling 911 for immediate help. Also, if you cannot get your child to drink or keep any fluids down, if they have severe abdominal pain or blood in their stool, you should call your doctor for guidance. And always -- You know your child best. Trust your gut (pun intended). If something about your child’s health status concerns you, do not hesitate to call your doctor.
We at Inspired Biometrics are committed to empowering parents to best care for their children through education and support. Check into www.inspiredbiometrics.com often for tips and educational posts.
Written by Rosey Olivero, MD
CSO and Co-Founder of Inspired Biometrics
09/29/19